نقش مهم „ویتامین دی„ برای بدن انسان. بویژه مبتلایان به اچ ای وی و بیماران ایدز
(for English text see below please!)
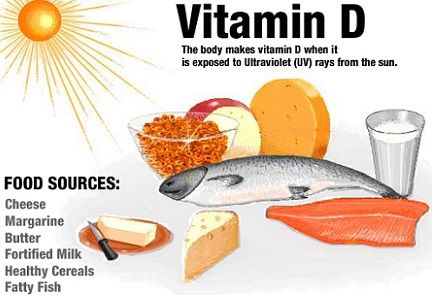 نور خورشید از جمله منبع اصلی تامین کننده ویتامین دی است و کمبود این ویتامین موجب شکل گیری امراضی از جمله دردهای استخوانی و عضلانی میشود
نور خورشید از جمله منبع اصلی تامین کننده ویتامین دی است و کمبود این ویتامین موجب شکل گیری امراضی از جمله دردهای استخوانی و عضلانی میشود
ویتامین «د» تنها نوع ویتامینی است که هورمون نیز محسوب میشود، این ویتامین برای محکم کردن استخوانها و همچنین به حفظ قدرت عضلانی و جذب کلسیم بدن کمک میکند
براساس پژوهشهای صورت گرفته، حدود 75 درصد از افراد مبتلا به ضعف عضلانی دچار کمبود ویتامین «د» هستند. همچنین تحقیقات نشان داده که کمبود ویتامین «د» خطر ابتلا به بیماریهای قلبی و عروقی را دو برابر افزایش میدهد و اشخاصی که میزان دریافت ویتامین «د» در آنها ضعیف است بییشتر از دیگران در معرض ابتلا به بیماری دیابت، چاقی و بیماریهای قلبی و عروقی قرار دارند
کسانی که داروهای ضد ویروس اچ آی وی استفاده میکنند نیاز بیشتری به مصرف ویتامین «د» دارندو. زیرا طی مطالعات و تحقیقات متعدد علمی تائید شده است که برخی از اثرات نامناسب جانبی این داروها بطور مثال تراوادا و یا داروهای پروتئاز موجب کمبود کلسیم و بیماریهای استخوانی و عضلانی در بدن مبتلایان می شوند
همچنین تحقیقات و پروژه های آزمایشی متعددی که تا سال 2014 میلادی در برخی کشورها مانند آلمان و آمریکا و .. انجام گرفته شده است نشان می دهد که تجویز و مصرف دوز های بالای ویتامین دی به مبتلایان اچ آی وی و بیماران ایدز تاثیرات بسیار مثبتی بر بدن وهمچنین از نظر روحی بر آنان داشته است
این آزمایشات تاکنون به تکرار کاملا نمایان و تائید کرده اند که ویتامین دی با دوزهای قوی نه تنها این بیماران را در برابر بیماری ساییدگی و آرتروز استخوانی و نیز بیماریهای قلبی مقاوم می کند, بلکه مبتلایان دارای سیستم ایمنی قوی تر و تعداد سلولهای کمکی بدن آنان بیشتر از سایر کسانی است که در این پروژه آزمایشی از ویتامین دی استفاده نکرده بودند. نکته بسیار پر اهمییت دیگر اینست که تعداد مرگ و میر در اینگونه بیمارانی که از ویتامین دی استفاده می کنند کمتر از مبتلایانی است که همواره از کمبود ویتامین دی در بدن برخوردارند
نوشتار: کیومرث سراج الهی
Vitamin D deficiency in HIV infection: an underestimated and undertreated epidemic.
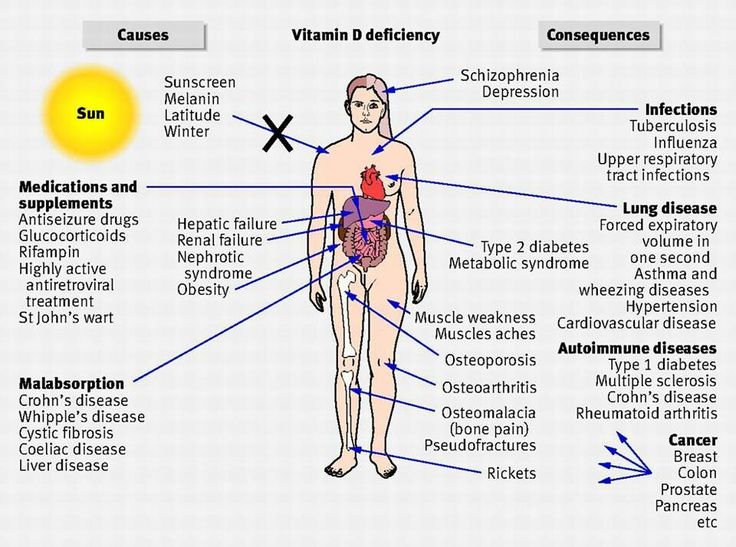 Hypovitaminosis D is a very common disorder, regarding both Western and developing countries. A growing amount of data over the last years have shown vitamin D deficiency to be high prevalent among HIV-positive subjects. In addition to „classic“ risk factors, such as female sex, low dietary intake, dark skin pigmentation and low sun exposure, HIV-related factors, including immune activation and antiretroviral adverse effects, may affect vitamin D status.
Hypovitaminosis D is a very common disorder, regarding both Western and developing countries. A growing amount of data over the last years have shown vitamin D deficiency to be high prevalent among HIV-positive subjects. In addition to „classic“ risk factors, such as female sex, low dietary intake, dark skin pigmentation and low sun exposure, HIV-related factors, including immune activation and antiretroviral adverse effects, may affect vitamin D status.
Even if both protease inhibitors and non-nucleoside reverse transcriptase inhibitors have been associated with low vitamin D levels, available evidences have failed to univocally associate hypovitaminosis D with specific antiretroviral class effects.
Low vitamin D is known to have a negative impact not only on bone health, but also on neurocognitive, metabolic, cardiovascular and immune functions. Similarly to the general population, several studies conducted on HIV-infected subjects have associated hypovitaminosis D with a greater risk of developing osteopenia/osteoporosis and fragility fractures.
Analogously, vitamin D deficiency has been described as an independent risk factor for cardiovascular disease and metabolic disorders, such as insulin resistance and type 2 diabetes mellitus.
Last EACS guidelines suggest to screen for hypovitaminosis D every HIV-positive subject having a history of bone disease, chronic kidney disease or other known risk factors for vitamin D deficiency. Vitamin D repletion is recommended when 25-hydroxyvitamin D levels are below 10 ng/ml.
Furthermore, it may be indicated in presence of 25OHD values between 10 and 30 ng/ml, if associated with osteoporosis, osteomalacia or increased parathyroid hormone levels. The optimal repletion and maintenance dosing regimens remain to be established, as well as the impact of vitamin D supplementation in preventing comorbidities.
Source: National Center for Biotechnology Information (NCBI)
Vitamin D deficiency associated with disease progression for patients with HIV
Vitamin D deficiency is highly prevalent in patients with HIV and is associated with an increased risk of disease progression, investigators from the EuroSIDA cohort report in the online edition of AIDS.
The investigators from Europe, Argentina and Israel found a strong relationship between low levels of the vitamin and an increased risk of all-cause mortality and the development of an AIDS-defining condition. They comment: “vitamin D deficiency therefore represents a new, independent, unfavourable prognostic marker in HIV infection.”
There is a some evidence showing that vitamin D deficiency is linked with a number of serious illnesses in the HIV-negative population, including cancers and heart disease, but the strongest association is between deficiency and bone thinning.
Levels of the vitamin below 10 nanograms per millilitre (ng/ml) are widely accepted as showing deficiency.
A number of studies have demonstrated that vitamin D deficiency is common in patients with HIV. Possible reasons include low levels of sun exposure, poor absorption, kidney or liver impairment, or the interference of antiretroviral drugs with vitamin D metabolism.
Investigators from the EuroSIDA cohort wished to establish the prevalence of vitamin D deficiency among their patients, its risk factors, and its relationship with disease progression.
A total of 1985 patients were involved in the study. Most of the patients (82%) were taking combination antiretroviral therapy.
Vitamin D levels were assessed on entry to the study, and placed into three categories: low (below 10 ng/ml); medium (10 to 30 ng/ml); and high (above 30 ng/ml).
Results showed that 24% of participants had vitamin D deficiency, 65% had moderate levels of the vitamin, and only 11% had vitamin D levels above 30 ng/ml.
“The present results confirm that vitamin D insufficiency or deficiency is frequent in HIV-infected persons,” comment the investigators.
For statistical reasons, the patients were then stratified into three categories (below 12 ng/m; 12 to 20 ng/ml and above 20 ng/ml).
Factors associated with vitamin D levels in the lowest tertile included black race (p = 0.0006), injecting drug use (p = 0.02), heterosexual HIV risk (p = 0.0001), and older age (p = 0.01).
HIV therapy that included a protease inhibitor was associated with a lower risk of vitamin D deficiency (p = 0.001). The investigators note this finding is “of unclear biological relevance”.
Next, the researchers examined the relationship between vitamin D levels and disease progression.
Five years after baseline, 10% of patients with vitamin D in the lowest tertile had developed AIDS, compared to 6% of individuals in the middle group and 5% of patients with the highest vitamin D levels.
Mortality rates also differed according to vitamin D status, and were highest for patients with vitamin D deficiency (11 vs 7 vs 6%). Rates of non-AIDS-defining events were 9 vs 7 vs 7%.
Low levels of vitamin D were related to poorer outcomes.
Compared to participants with the lowest levels of vitamin D, people in the middle and upper tertiles had a significantly lower risk of progression to AIDS (p = 0.00086 and p = 0.02 respectively).
Similarly, the risk of death was lower for people in the middle and upper tertiles (p = 0.045 and p = 0.003 respectively).
People with the highest levels of vitamin D were also significantly less likely than those with vitamin levels below 12 ng/ml to die of a non-AIDS-related cause.
Adjustment for CD4 cell count and viral load further confirmed that patients with moderate or high levels of vitamin D had a reduced risk of death (p = 0.025 and p = 0.048 respectively).
“A very low [vitamin] D level was associated with events, even in the case of virologically controlled HIV infection and immune restoration,” the authors emphasise.
They conclude: “These results provide strong evidence that vitamin D deficiency is an important cofactor in HIV disease progression, even in the setting of widespread, efficient cART [combination antiretroviral therapy]. Whether the relationship between vitamin D deficiency and events is casual must now be addressed.”
Source: aidsmap